Imagine a world where we can effortlessly capture and interpret the intimate core of our bodily functions without invasive procedures or bulky devices. Envision a perfect harmony between technological innovation and simplicity, enabling us to gain insightful knowledge about our body's thermoregulation process with a single, discreet gesture. This captivating vision is not a distant reverie but a plausible reality on the horizon.
Enter the realm of temperature assessment beneath the arm, a captivating approach that holds the promise of tapping into the body's inner workings discreetly. Within every corner of this fascinating exploration lies a treasure trove of information waiting to be unearthed. Through the use of advanced engineering and cutting-edge sensors, this unassuming part of our anatomy becomes a window to understanding our physiological state.
Delving deeper, one is mesmerized by the profound implications of this innovative method. By delicately embracing the concept of thermoregulation and guiding our comprehension towards a more profound understanding of our body's unique language, we unlock the potential for preventative healthcare measures, early detection of underlying conditions, and personalized wellness management.
The significance of such a breakthrough extends far beyond mere convenience. By probing beneath the arm's surface and skillfully extracting data, this non-invasive method offers a gateway to a more connected healthcare experience. It paves the way for a future where individuals can effortlessly monitor their health without interrupting their daily routines, empowering them to take proactive steps towards their well-being with ease and confidence.
A Fresh Approach to Monitoring Body Heat
Innovation knows no bounds when it comes to temperature tracking methods. In this unique exploration, we delve into a novel perspective on the subject, steering clear of conventional approaches and focusing on alternative ways of gauging body heat levels. By offering an alternative lens, we aim to broaden the horizons of temperature monitoring techniques, paving the way for new insights and advancements.
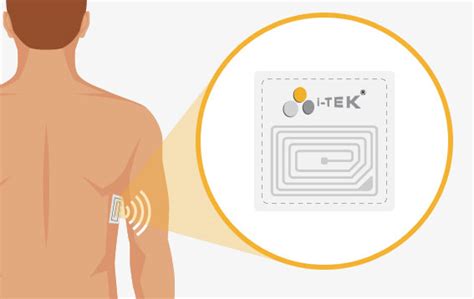
1. Utilizing Cutting-Edge Sensors: Relying on state-of-the-art sensor technology, this approach takes advantage of modern advancements in temperature detection. By harnessing the power of these sophisticated sensors, we unlock a new realm of precision and accuracy in measuring and monitoring body heat.
2. Exploring Alternative Placement: Opting for a less commonly used location for temperature readings, this approach introduces a fresh perspective. By exploring alternative areas such as the axillary region or other strategic points, we can obtain valuable temperature data without compromising comfort or convenience.
3. Embracing Wireless Connectivity: Breaking free from traditional wired connections, this approach embraces the possibilities of wireless technology. From Bluetooth-enabled sensors to smart devices, the convenience of wireless connectivity empowers users to effortlessly track and analyze body temperature on various platforms and devices.
- A holistic approach to temperature monitoring
- Enhanced precision and accuracy
- Increased user comfort and convenience
- Potential for real-time data analysis
- Expanded applications in healthcare and beyond
As we venture beyond the realm of conventional temperature measurement, possibilities unfold and pave the way for exciting innovations in healthcare, wellness, and daily life. By embracing this fresh approach to monitoring body heat, we set the stage for a new era of temperature tracking, revolutionizing the way we understand and respond to changes in our bodies. With endless potential waiting to be realized, it is time to embark on this journey towards a more comprehensive understanding of body temperature.
Exploring the Armpit as a Trustworthy Alternative
The armpit, an often overlooked area of the body, holds great potential for accurate temperature measurement without the need for invasive or uncomfortable methods. This section aims to explore the armpit as a reliable alternative to conventional temperature measuring techniques, offering a deeper understanding of the benefits it can provide.
Non-invasive and Comfortable By utilizing the armpit as a measuring site, individuals can experience a non-invasive and comfortable method of temperature assessment. Unlike oral or rectal measurements, which may cause discomfort or distress, placing a thermometer under the arm offers a more pleasant experience for both adults and children. | Affordable and Accessible Measuring temperature under the armpit requires no expensive or specialized equipment. Most modern digital thermometers are equipped with underarm temperature measurement capabilities, making this method easily accessible to a wide range of individuals. This affordability and accessibility contribute to the practicality of using the armpit as an alternative measuring site. |
Consistency and Accuracy Scientific studies have shown that armpit temperature measurements can provide consistent and accurate results. With proper positioning and technique, the armpit can offer a reliable reflection of the body's internal temperature. This consistency is crucial in medical settings to monitor and manage various conditions effectively. | Convenient and Hygienic Taking temperature under the armpit requires minimal preparation and can be performed anywhere. It eliminates the need for special clothing or privacy, making it a convenient method for quick and frequent temperature checks. Additionally, the armpit is easily accessible for self-measurement and poses no hygiene concerns when using disposable probe covers. |
By exploring the armpit as a trustworthy alternative to traditional temperature measurement methods, we open doors to more comfortable, accessible, and accurate practices. Its convenience, affordability, and reliability make it a valuable option for both medical professionals and individuals seeking to monitor their body's temperature effectively.
The Importance of Precise Body Temperature Assessment
Accurate measurement of body temperature plays a vital role in diagnosing and monitoring various health conditions. Obtaining precise temperature readings allows healthcare professionals to make informed decisions regarding patient care and treatment. Reliable temperature assessment not only aids in identifying and managing infectious diseases but also assists in assessing the efficacy of interventions and evaluating overall wellness.
Precise body temperature measurement facilitates the early detection of conditions such as fever, hypothermia, and other abnormal fluctuations. It enables healthcare providers to promptly intervene and initiate appropriate treatment measures, preventing potential complications. Additionally, accurate temperature assessment aids in monitoring body responses and identifying patterns that may indicate underlying health concerns.
The significance of accurate body temperature measurement extends beyond clinical settings. It is equally crucial in assessing the effectiveness of therapeutics and medical devices. Accurate temperature readings contribute to the development and refinement of temperature-sensitive treatments, optimizing their impact on patients and enabling personalized care.
Furthermore, precise body temperature assessment enhances the accuracy of research studies and clinical trials. Reliable temperature data empowers researchers to draw well-founded conclusions, providing valuable insights into the effectiveness of interventions, the progression of diseases, and the impact of environmental factors on human health.
The measurement of body temperature relies on various approaches, including oral, rectal, tympanic, and axillary methods. Each technique offers distinct advantages and limitations, with the armpit being a widely accessible and non-invasive site for temperature measurement. Ensuring precise measurements not only improves the reliability of temperature readings but also enables consistent comparisons across different measurement methods.
In conclusion, accurate body temperature measurement is of paramount importance in healthcare, research, and therapeutic development. By obtaining precise temperature readings, healthcare professionals can effectively diagnose and manage various health conditions, while researchers can acquire reliable data for evidence-based conclusions. Therefore, investing in innovative and reliable temperature assessment methods ultimately benefits individuals, healthcare providers, and the advancement of medical knowledge.
Why Precise Data Matters in Healthcare and Beyond
In today's rapidly advancing world, precise data plays a critical role in various sectors, including healthcare. The ability to obtain accurate and detailed information is paramount, as it directly impacts the quality of care, effective decision-making, and advancements in medical research.
Reliable data enables healthcare professionals to make informed diagnoses, monitor patient progress, and develop personalized treatment plans. By having access to precise data, doctors can better understand the intricacies of an individual's health, leading to improved outcomes and a higher level of patient satisfaction.
Moreover, precise data also serves as a catalyst for advancements in healthcare technology and innovation. By relying on accurate information, researchers can identify patterns, trends, and potential areas for improvement. This fuels the development of new medical devices, pharmaceuticals, and treatment methods, ultimately leading to better healthcare outcomes for individuals worldwide.
Not limited to healthcare alone, the importance of precise data extends to other industries as well. In the field of education, accurate data allows educators to identify areas of student weakness, tailor teaching methods, and measure educational progress effectively. In the realm of business, precise data enables companies to make informed decisions, identify market trends, and optimize operations for enhanced efficiency and profitability.
In conclusion, the significance of precise data cannot be overstated. Whether in healthcare or in other sectors, it serves as the foundation for progress, innovation, and informed decision-making. By harnessing the power of accurate and detailed information, we can drive meaningful advancements that impact the lives of individuals and society as a whole.
Practical Challenges and Inherent Limitations of Conventional Approaches
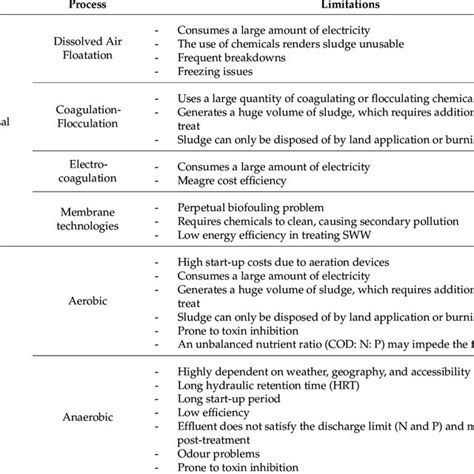
When it comes to assessing the body temperature in a non-invasive manner, the traditional methods employed face various challenges and limitations. These obstacles can hinder their effectiveness and accuracy, thereby impacting the overall reliability of temperature measurements. Recognizing these shortcomings is crucial for the development of more advanced and reliable techniques.
One of the primary challenges associated with conventional methods is the inherent variability resulting from human factors. Factors such as individual differences in body composition, clothing, and ambient temperature can significantly affect the accuracy and consistency of temperature measurements. Moreover, external factors like humidity and perspiration can further complicate the interpretation of results.
Additionally, the traditional approaches often require direct contact with the skin's surface, which may not always be practical or comfortable. This limitation can be particularly relevant in situations where frequent temperature monitoring is necessary, such as in healthcare settings or during athletic activities. The discomfort caused by repeated contact can lead to inconsistent measurement practices and inaccurate results, undermining the purpose of temperature assessment.
Moreover, the reliance on conventional thermometers often necessitates the need for user compliance and cooperation. Ensuring consistent and accurate readings becomes challenging when factors like patient discomfort or reluctance come into play, especially with certain demographics such as children or individuals with sensory sensitivities.
Another significant limitation lies in the time required for measuring temperature using traditional methods. In many cases, the process involves waiting for several minutes to obtain an accurate reading, which can be impractical, especially in scenarios where quick and efficient evaluation is crucial. This time-consuming approach may impede timely interventions and thereby jeopardize the effectiveness of temperature management strategies.
In conclusion, the traditional methods employed for measuring body temperature face several challenges and limitations that compromise their effectiveness and practicality. Addressing these issues is imperative for the development of innovative and more reliable approaches that can improve the accuracy, comfort, and efficiency of temperature assessment.
Examining the Limitations of Oral and Rectal Thermometers
In this section, we will explore the drawbacks associated with using oral and rectal thermometers for measuring body temperature. While these conventional methods have long been relied upon, it is important to acknowledge that they are not without their limitations. By understanding the shortcomings of these thermometer types, we can better appreciate the need for alternative temperature measurement techniques.
- 1. Invasiveness:
- 2. Variability in Measurement:
- 3. Hygiene Concerns:
- 4. Challenging for Certain Populations:
- 5. Lack of Convenience:
Both oral and rectal thermometers require direct contact with the mucous membranes or rectal area, which can cause discomfort or pose potential health risks. This invasiveness may deter individuals, particularly children or those with certain medical conditions, from adhering to regular temperature monitoring.
Oral and rectal thermometers are prone to variations in measurement due to external factors such as eating, drinking, or smoking, which can affect oral temperature, and recent bowel movements, which can influence rectal temperature. These factors can hinder the accuracy and consistency of temperature readings.
Both oral and rectal thermometers require proper cleaning and disinfection after each use to prevent the transmission of germs and infections. Failing to maintain hygiene practices can lead to cross-contamination and compromised accuracy of subsequent measurements.
Oral temperature measurement can be difficult for young children or individuals with conditions that affect their ability to hold the thermometer under their tongue. Similarly, rectal temperature measurement poses challenges for individuals with rectal conditions or those who may find the process uncomfortable or embarrassing.
Both oral and rectal thermometers generally require an appropriate location for temperature measurement, making it inconvenient for individuals who may be immobile or unable to access a suitable environment for the procedure. Additionally, achieving accurate measurements may require longer waiting times, which can be inconvenient for individuals seeking quick and efficient temperature monitoring.
By understanding the limitations associated with oral and rectal thermometers, we can recognize the importance of exploring alternative methods, such as non-invasive armpit temperature measurement, which offers greater comfort, simplicity, and ease of use.
FAQ
Why is measuring body temperature under the armpit important?
Measuring body temperature under the armpit is important because it provides a non-invasive and easy way to monitor our body's health. It is particularly useful for parents who need to measure their child's temperature, as it can be less intrusive and more comfortable than other methods.
How accurate is measuring body temperature under the armpit?
Measuring body temperature under the armpit is generally considered to be less accurate than other methods, such as measuring orally or rectally. It provides a rough estimate of body temperature with a slightly lower reading, as the armpit is not as closely correlated to our core body temperature. However, it can still be a useful indicator of any potential fever or change in body temperature.
Can measuring body temperature under the armpit be used for medical diagnosis?
While measuring body temperature under the armpit can give a general indication of body temperature, it is not typically used for medical diagnosis. Healthcare professionals usually prefer more accurate methods, such as rectal or oral measurement, for diagnosing and monitoring illnesses. However, underarm temperature measurement can still be helpful for initial assessment or at-home monitoring.
Are there any disadvantages to measuring body temperature under the armpit?
Measuring body temperature under the armpit has a few disadvantages. First, it is generally less accurate than other methods. Secondly, it may take longer to get an accurate reading compared to oral or rectal measurement. Additionally, factors such as sweating or clothing can affect the accuracy of the measurement. While it can be convenient in certain situations, it's important to consider these limitations when using this method.




